The World Health Organization observes October 10th as World Mental Health Day in an effort to increase public awareness of mental health-related concerns. The annual campaign support the battle to reduce stigmas associated with mental illness and to ensure that mental health services are available to everyone by fostering conversations about mental health issues. WHO encourages people to accept responsibility for mental health problems, seek every possible assistance when needed, and push for governments to put mental health on the public agenda.
With all these initiatives, mental health is still in the Indian subcontinent generally a very vaguely defined and neglected area. The views, treatments as well as the discussions pertaining to mental health were considered pretty much diversely by different regions and social setups despite more significant advances in education, wide-ranging awareness efforts, and expanded discourses on mental health. On one hand, it is written off as something paranormal. Thus instead of receiving the treatment needed, people seek an antidote in the form of superstition. On other, words like "stress," "anxiety," and "depression" often misused and applied carelessly, lessens the severity of mental illnesses. Their relevance and purpose will be lost as a result of this trend. The term "depression" is widely applied to any type of stress or emotional low, diminishing the seriousness of the condition and discouraging individuals who genuinely suffer from it from seeking treatment.
The Indian subcontinent's cultural fabric is closely linked to tradition, which prioritizes physical health over emotional and mental well-being. This is primarily due to a lack of knowledge about psychological disorders and the belief that emotional difficulties should be suppressed. It is still taboo to discuss mental health in conservative societies and rural areas. They suffer in quiet because it's seen as a family embarrassment for some.
Many people believe that mental illnesses are caused by spiritual imbalances, black magic, or karmic misalignments. They view obtaining professional mental health assistance as completely unnecessary, even disgraceful, due to the stigma associated with it. Family members frequently wish to disregard symptoms or pursue home remedies rather than consulting a scientist, which delays treatment until later.
It is true that in both the rural and urban scenario, people tend to trivialize their problems relating to mental health until such problems acquire a serious form. This is perhaps because they wait for the patient to present some markedly grave manifestations of depression, anxiety, or even psychosis. The main reason for the delay is that most people are typically unable to identify the early warning signs of mental health decline. For instance, behavioral changes, mood swings, social disengagement, or extreme irritation are typically dismissed as transitory phenomena rather than warning signs of a problem.
The poor mental health literacy exacerbates the matters. Even in developed cities, most places in this subcontinent are illiterate or ignorant about what role mental health plays in determining the overall well-being of the individual. Moreover, institutional efforts at improving mental health knowledge and screening and intervention programs in schools and even in corporate segments that lead to late detection and treatment are lacking.
Indian urbanization is undoubtedly on the rise with a fast pace that involves both economic and sociocultural changes. Societal and economic changes happening around the world influence the mental health syndrome of people and exert stringent pressure on their mental well-being. Increasing stress in every level of life, problems of modern living and disorganization in the family system are among the contributing factors toward mental health disorders. It really does affect how people perceive the way relationships or success should be or how a perfect body should look. Together, all these hangings create fear and low self-esteem.
Urbanization has brought about tremendous changes in the work patterns. An increase in working hours, disconnection of persons, high cost of living, and overarching pressure to act in tune with social demands have all contributed to aggravating the scale of stress-related diseases. The recent deaths of two workers due to work-induced stress are only a sign of what is looming large to unfold in the terms of mental illness at the workplace.
According to the estimates by World Health Organization, some 13% of the total population in the world suffers from mental health problems, thus making it one of the biggest contributors towards disability in this world today. It is reported that around 7.5% of the population of India is estimated to be suffering from mental health issues that greatly put pressure on people individually and on the society as a whole. The socio-economic challenges that will be accompanied by politically unstable circumstances are expected to increase the levels of mental health disorders in years to come.
Some 3.8% of people have ever experienced depression, with approximately 5.7% among those aged 60 and older and 5% of adults (4% among men and 6% among women). Depression affects about 280 million people worldwide. Women are around 50% more likely than men to experience depression. More over 10% of expectant mothers and recent mothers experience depression globally (2). An estimated 700,000 people lose their lives to suicide each year. The fourth most common cause of mortality for people aged 15 to 29 is suicide. 1 in every 8 people in the world live with a mental disorder
Mental health is usually the least priority of governments. It is still an article of faith that India had launched its first National Mental Health Policy as far back as 2014 and the Mental Healthcare Act that came into effect in 2017, but implementation is meager. Mental health professionals are in acute shortage at less than one psychiatrist available per 100,000 people. This gap merges with insufficient funding for mental health infrastructure, hence the difficulty that citizens face in acquiring timely and affordable services in their mental health.
It is estimated that one-fifth of Indians may suffer from some kind of mental illness during the course of their lifetime and within the country itself, which bears 15 percent of the global burden of disease related to mental health issues. As per the report submitted by NIH, suicide rate in 2022 is 11.6 and as marked exponentially on the growth scale. Within a short period of years, depression alone will probably emerge as the second-largest and third-largest contributor to disease burden in low and middle-income nations, respectively, by 2030. The report further states, “Despite this dire need, the Indian government spends only about 0.06 per cent of its total health expenditure on mental health, with only 0.75 psychiatrists per 100,000 people, and even lesser on mental health nurses, social workers and psychologists. Moreover, lack of mental health awareness continues to be a major issue in rural areas and disadvantaged strata of the society. For example, 64.2 per cent of suicides were amongst those earning an annual income of less than ₹ 1 Lakh.While nearly 200 million Indians would benefit from mental health services, fewer than 30 million seek care because access is limited and stigma often prevents them from seeking help.
Indian socio-politics worsened the mental health condition in the country. This region is facing alarming identity disputes and political, economic unrest that has caused widespread anxiety and emotional pain. The stress and trauma people go through lead to increased mental health disorders in areas caught in the turmoil of violence, social confusion, and political unrest.
Breaking the taboo about mental health in India is highly multi-dimensional. To begin with, awareness programs need to be initiated, enlightening them about the significance of well-being in one's brain and the myths associated with mental illness. Communities, particularly rural areas, are to be allowed to talk and concentrate upon their mental health issues. Simultaneously, urban population needs to be made aware and charged with the responsibility of handling mental health terms properly and realizing that how serious these diseases may turn out to be.
The government and NGOs must work towards building a strong mental health infrastructure, thereby training more mental health professionals and developing affordable and accessible treatment facilities. Mental health education would be part of any school curriculum and mental health policies would be implemented to ensure early intervention in the workplace.
Let the Truth be known. If you read VB and like VB, please be a VB Supporter and Help us deliver the Truth to one and all.
Ottawa (PTI): Three Indian nationals have been arrested by Canadian police on an anti-extortion patrol and charged after bullets were fired at a home.
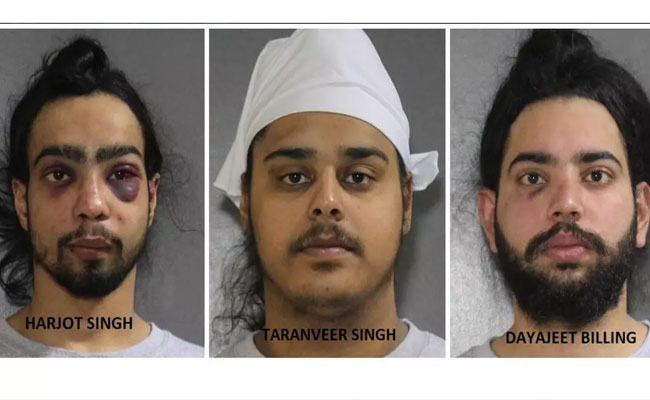
Harjot Singh (21), Taranveer Singh (19) and Dayajeet Singh Billing (21) face one count each of discharging a firearm, and all have been remanded in custody until Thursday, the Surrey Police Service (SPS) said in a statement on Monday.
The suspects were arrested by patrol officers after an early morning report of shots fired and a small fire outside a home in Surrey's Crescent Beach neighbourhood, the LakelandToday reported.
On February 1, 2026, the SPS members were patrolling in Surrey’s Crescent Beach neighbourhood when reports came in of shots being fired and a small fire outside a residence near Crescent Road and 132 Street.
The three accused were arrested by SPS officers a short time later, the statement said.
SPS’s Major Crime Section took over the investigation, and the three men have now been charged with Criminal Code offences, it said.
All three have been charged with one count each of discharging a firearm into a place contrary to section 244.2(1)(a) of the Criminal Code.
The investigation is ongoing, and additional charges may be forthcoming. All three have been remanded in custody until February 5, 2026.
The SPS has confirmed they are all foreign nationals and has engaged the Canada Border Services Agency, it said.
One of the suspects suffered injuries, including two black eyes, the media report said.
Surrey police Staff Sgt. Lindsey Houghton said on Monday that the suspect had refused to comply with instructions to get out of the ride-share vehicle and started to "actively resist."
"As we were trained, he was taken to the ground and safely handcuffed," said Houghton.
A second suspect with a black eye was also injured in the arrest after refusing to comply, Houghton said.
The arresting officers were part of Project Assurance, an initiative that patrols neighbourhoods that have been targeted by extortion violence.
Houghton said the Canada Border Services Agency (CBSA) is also involved because the men are foreign nationals, and the trio may face additional charges.
It's not clear if the men are in the country on tourist visas, a study permit, or a work permit, but Houghton said CBSA has started its own investigation into the men's status.
Surrey has seen a number of shootings at homes and businesses over the last several months, but there's been an escalation since the new year.